In the years following your first knee replacement surgery, the metal portion of your implant slowly wears down this plastic portion.
Depending on the amount of wear to this plastic piece, your surgeon may be able to replace only the plastic piece alone. In other cases, though, you may have worn through it and damaged the metal components as well. In this case, the entire implant will be replaced.
Why you might need knee revision surgery
Osteolysis
The wearing down of the plastic component has an unfortunate side effect. The tiny plastic particles that wear off are attacked by your body’s immune system, and this immune response also attacks the healthy bone around your implant. This leads to a condition called osteolysis, in which the bone in the area around the joint implant softens as it is absorbed by the body, thus making your implant unstable and in need of revision. Your consultant orthopaedic surgeon usually will be able to detect osteolysis on your standard X-rays.
Fracture
If the bone next to your primary implant is fractured in an accident, revision surgery may be required in order to provide a safe, stable joint. In this case, the original implant may need to be removed, the fracture addressed and a revision joint implanted.
Infection
In a low percentage of cases, your knee may become infected after surgery. Although it may be successfully treated with antibiotics, there are severe cases where a follow-up revision surgery may be required. In this surgery, the primary implants will be removed, and temporary, antibiotic-laced “spacers” are implanted. These spacers allow for joint function and are intended to give your body time to heal before the new revision prostheses are surgically implanted. Most likely, you will be put on a six-week course of antibiotics in order to eliminate the infection. At a follow-up evaluation, your surgeon will determine if your body is ready for the revision procedure.
The Implant
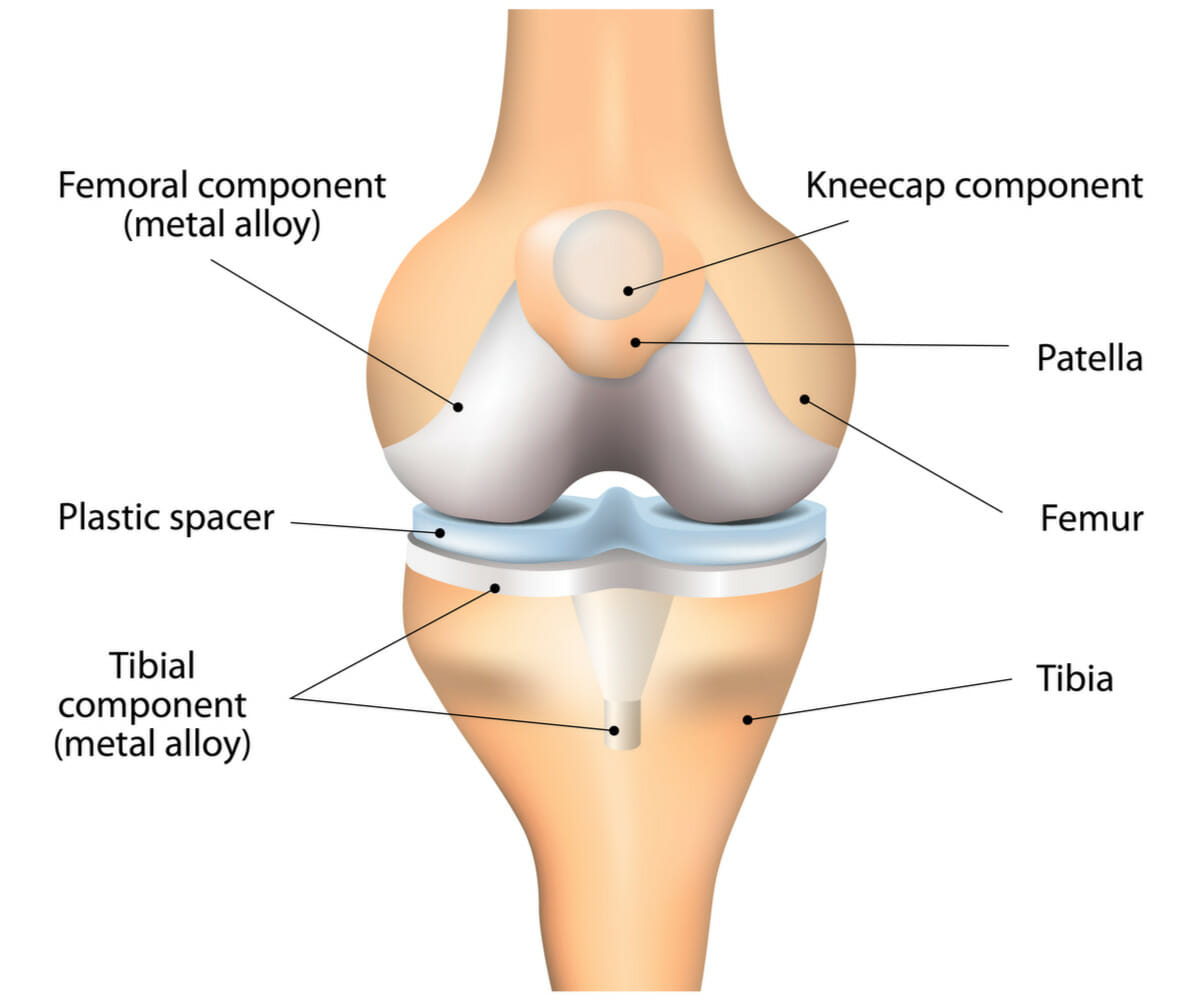
In revision knee surgery, each prosthesis is made up of four parts. The tibial component has two elements and replaces the top of the shinbone (tibia). This prosthesis is made up of a metal tray attached directly to the bone and a plastic spacer that allows the thighbone to move over the shinbone.
The femoral component replaces the bottom of the thighbone (femur). This component also replaces the groove where the kneecap (patella) sits. The patellar component replaces the undersurface of the kneecap, which rubs against the thighbone. The kneecap protects the joint, and the resurfaced patellar component slides smoothly on the front of the joint.

Information leaflet
This document is intended for information purposes only and should not replace advice that your relevant health professional would give you.
© EIDO Systems International
The operation and treatment information on this webpage is produced using information from EIDO Systems International and is licensed by Horder Healthcare. The information should not replace the advice that your relevant health professional would give you.
Consultants that perform this procedure
Get referred to The Horder Centre today
The Horder Centre provides the highest quality services to NHS, privately insured and self-pay patients, from initial consultation and diagnostic tests right through to surgical treatment and rehabilitation.
We are rated as a 5* healthcare provider
Read our latest patient reviews on the NHS Choices website.












